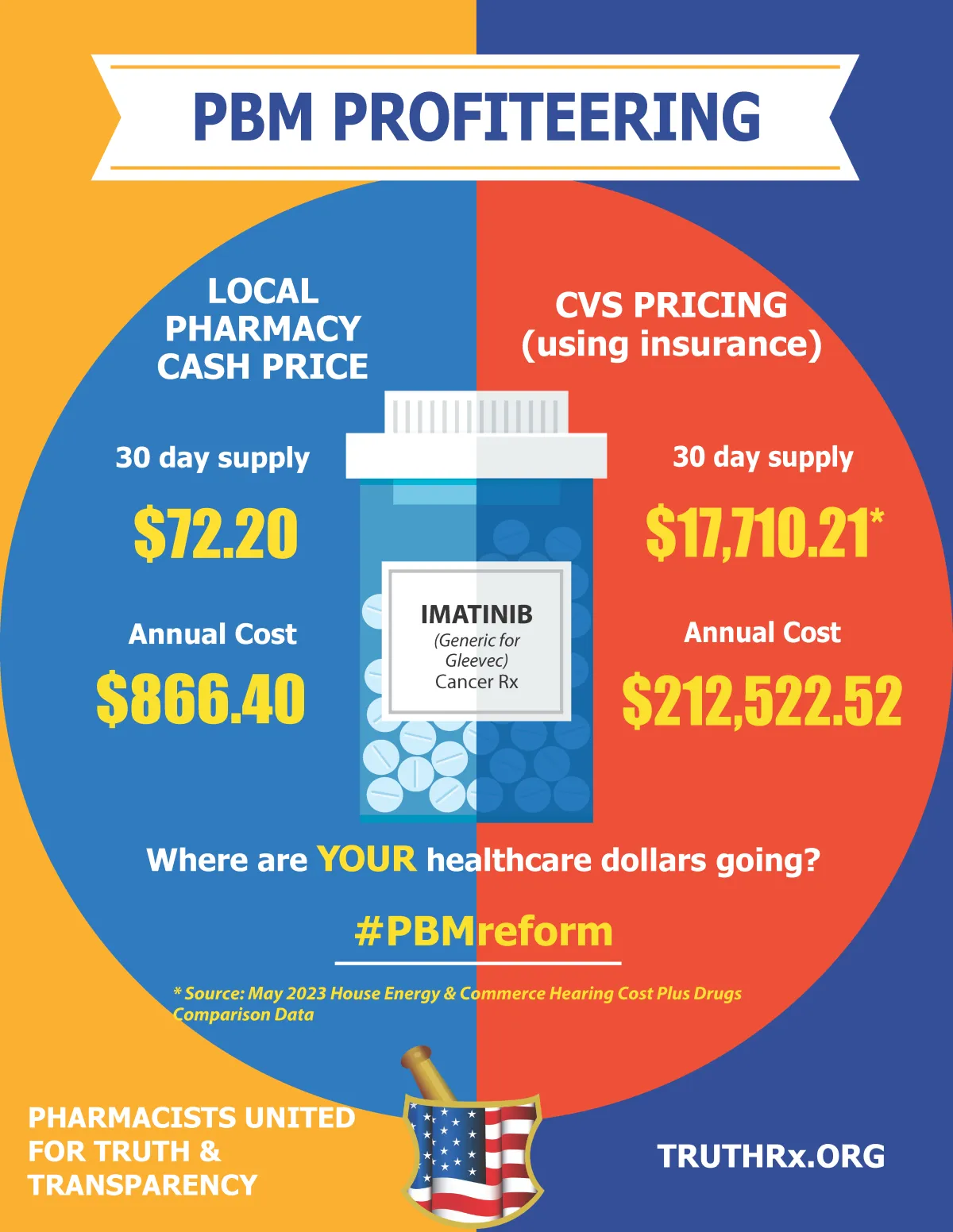
The Pharmacy Benefit Manager (PBM) Problem
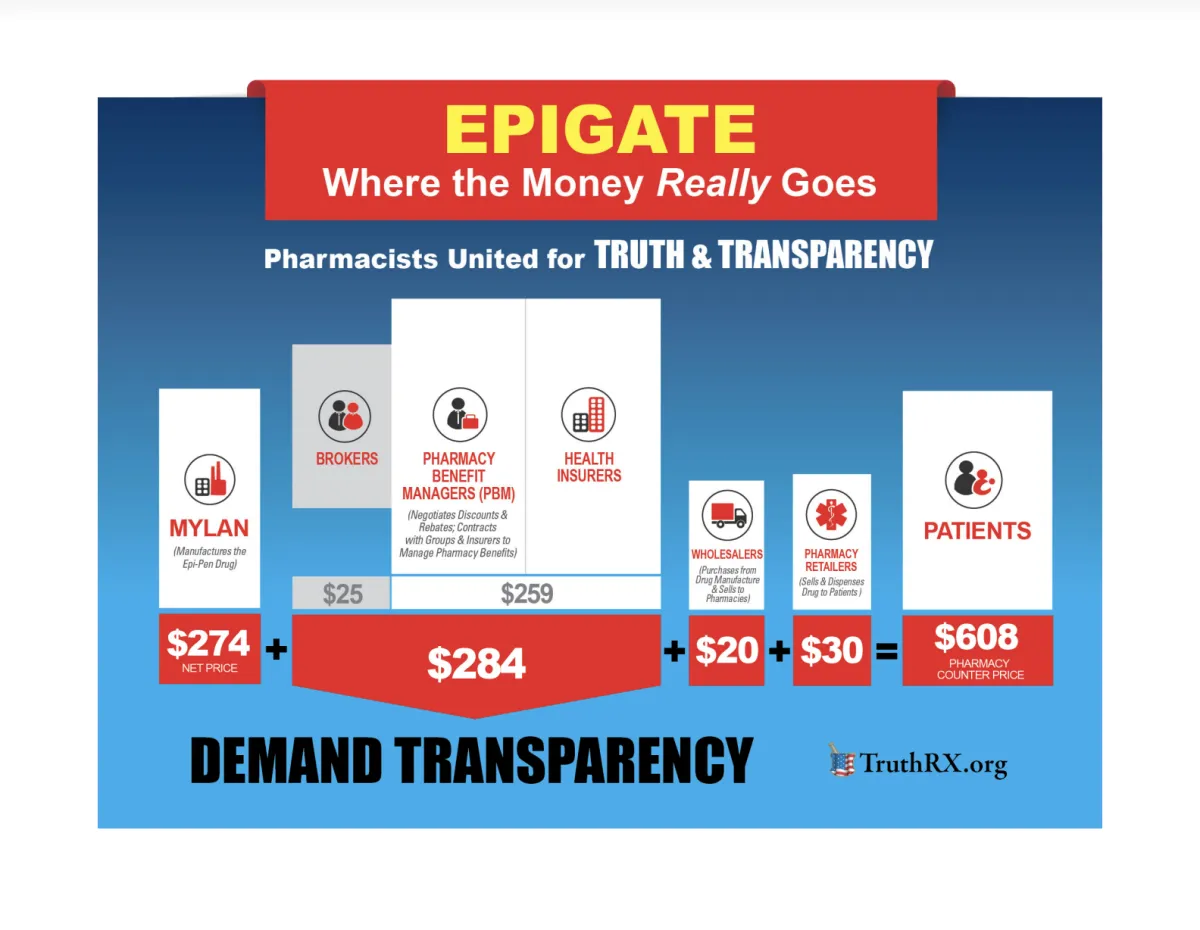
Pharmacy Benefit Managers (PBMs) are middlemen.
In pharmacy, PBMs are hired by entities that pay for patients' health insurance (for example, private insurance companies, TRICARE, Medicare, and state Medicaid programs) to "manage" patients' prescription drug benefit.
First and foremost, this involves the electronic processing of prescription claims* (which happens when a pharmacy fills a patient's prescription using their insurance), but now also includes several other responsibilities:
Creating the "formulary" of covered drugs for payers
(i.e., they’re the reason your medication is covered, your prescription requires a PA, or why you have
to take the expensive brand-name version of a medication when a cheaper generic version exists)
Negotiating rebates with drug manufacturers
(i.e., they have a financial incentive to create formularies that include those manufacturer’s drugs)
Creating pharmacy networks
Reviewing drug utilization
Managing mail order specialty pharmacies
(i.e., they’re the reason that mail order pharmacies are cumbersome to work with, to the point of significantly negatively impacting patients’ care experience (sometimes even in outright unethical ways))
*They’re the reason the billing of your prescriptions is increasingly convoluted, putting greater logistical burden on patients, providers, and payers
WATCH and learn
PBM abuse IN THE NEWS







Contact Us
Site has Been Created and Operated by Justice for Cole and All Others LLC